Genetics 101
Cells are the fundamental working units of every living system. All the instructions needed to direct their activities are contained within the DNA that resides in the cell’s nucleus.
Below you’ll find a tutorial to answer your most frequently asked questions.
The Basics
DNA from all organisms, from the tiniest bacteria to humans, is made up of the same chemical and physical components. The DNA is organized like a twisted ladder with bonds between the rungs that can be “unzipped” like a zipper. The rungs are made up of nucleotide bases called A,C,T, and G. A always pairs with T and C always pairs with G. This order spells out the exact instructions required to create a particular organism with its own unique traits.
The genome is an organism’s complete set of DNA. Genomes vary widely in size: the smallest known genome for a free-living organism (a bacterium) contains about 600,000 DNA base pairs, while human and mouse genomes have some three billion. Each human cell contains a complete genome.
DNA in the human genome is arranged into 23 chromosomes, each containing many genes. The X and Y chromosomes determine the sex of a baby. Girls have two X chromosomes and no Y, and boys have one X and one Y. The MECP2 gene is located on the X chromosome. Girls with Rett therefore have two MECP2 genes, one that is mutated and one that is normal.
Although genes get a lot of attention, it’s the proteins they encode that perform most life functions, and even make up the majority of cellular structures. Proteins are large, complex molecules made up of many subunits called amino acids. Chemical properties that distinguish the 20 different amino acids cause the protein chains to fold up into specific three-dimensional structures, which define their particular functions in the cell.
Decoding DNA
A single strand of DNA is made of letters:
A T G C T C G A A T A A A T G T G A A T T T G A
Every 3 letters make up a word, also known as amino acids. Many words together make up a gene. The MECP2 protein is made up of almost 500 amino acids.
ATG CTC GAA TAA ATG TGA ATT TGA

MECP2 Mutations
What it Means
A gene mutation is a permanent change in the DNA sequence. Mutations range in size from only one nucleotide base to a large segment of DNA comprising many genes.
By changing a gene’s instructions for making a protein, a mutation can cause the protein to malfunction or to be missing entirely. In Rett syndrome, a mutation in the MECP2 gene causes the MECP2 protein to be mutated as well.
It is important to note that genes themselves do not cause disease – genetic disorders are caused by mutations that make a gene function improperly. For example, when people say that someone has “the Rett Syndrome gene,” they are referring to a mutated version of the MECP2 gene, which causes the disorder. All people, including those without Rett syndrome, have an MECP2 gene.
Your child’s results usually contain two pieces of information – a number that refers to which nucleotide base is mutated, and a number that corresponds to the resulting change in the amino acid sequence.
You may also be told that the mutation is heterozygous, meaning your daughter has one normal X chromosome and one X chromosome with a mutated MECP2. Boys with MECP2 mutations are homozygous because they have only one X chromosome. Below are some examples of typical mutations.
Girls with Rett have a healthy copy of the gene in every one of their cells alongside the mutated one but the healthy gene is silent about 50% of the time. We’re funding research to activate the healthy cells which, in theory, could be a cure!
Types of Mutations
Missense Mutation
This type of mutation is a change in one DNA base pair that results in the substitution of one amino acid for another.
Example: 473 C –> T / T158M
The first number refers to the nucleotide base that is mutated. In this particular case, at nucleotide base number 473 there should have been a cytosine nucleotide base, but due to the mutation there is now a thymine.
This results in a different amino acid being encoded. At amino acid number 158 (divide 473 by 3 to get the amino acid number, since every three bases encode for an amino acid) there should have been a threonine but there is now a methionine. This simple change of only one amino acid out of almost 500 amino acids makes the protein dysfunctional.
Nonsense Mutation
A nonsense mutation is also a change in one DNA base pair. Instead of substituting one amino acid for another, however, the altered DNA sequence prematurely signals the cell to stop building a protein. This type of mutation results in a shortened protein that may function improperly or not at all.
Example: R168X [The X denotes a mutation that results in a prematurely truncated protein.]
Missense Mutation
An insertion changes the number of DNA bases in a gene by adding a piece of DNA resulting in a dysfunctional protein.
Example: 620insT [At nucleotide base number 620 an extra thymine was inserted.]
Deletion
A deletion changes the number of DNA bases in a gene by removing a piece of DNA. The deleted DNA alters the function of the resulting protein.
Example: 803del4 [At nucleotide base number 803, four bases were deleted.]
Frameshift Mutation
This type of mutation occurs when the addition or loss of DNA bases changes a gene’s reading frame. A reading frame consists of groups of three bases that each code for one amino acid. A frameshift mutation shifts the grouping of these bases and changes the code for amino acids. The resulting protein is usually non-functional. Insertions, deletions, and duplications can all be frameshift mutations. The 620insT and 803del4 examples above both result in frameshift mutations.
Other Important Questions
Most females have a random inactivation pattern which activates roughly 50% of one X and 50% of the other chromosome. However, for reasons unknown, it can happen that a female will skew one X over the other. If a girl favors inactivation of the X with the mutated MECP2, she will have less severe symptoms. If the reverse happens the child may have more severe symptoms.
Although it is possible to test the X inactivation pattern in blood it is not possible to know the pattern where it counts, in the brain, so the clinical usefulness of testing is limited.
Another variable is the child’s own genetic make-up that may influence the severity of symptoms.
A number of studies attempting to correlate specific mutations to symptoms have yielded inconsistent results. Some very general conclusions include:
- The R133C mutation, as well as missense mutations are typically mild
- Truncating mutations appear to correlate with breathing abnormalities whereas scoliosis was more common in individuals with missense mutations
- Early truncating mutations have a more severe outcome than late truncating or missense mutations
It’s important to note that these are generalizations based on large sample sizes. Drawing conclusions regarding your child’s mutation on a case-by-case basis is not reliably predictive.
The vast majority of mutations are sporadic, not familial, and originate from a mutated sperm. In such cases, a father, if tested for MECP2 mutations, will test negative since he does not have mutations in any of his cells except for the particular sperm which fertilized the egg that resulted in his daughter.
In families where MECP2 mutations have been identified in more than one family member, there are two possible explanations:
- The mother has an MECP2 mutation but has favorably skewed her X inactivation pattern so she is asymptomatic
- The mother has mutations in her eggs but in no other tissue. She is therefore completely symptom free but has a 50% chance of passing the mutation on to her offspring. This is called germline mosaicism
Males and Rett Syndrome
With the exception of activating the silent MECP2, all of the research that RSRT supports is as relevant to boys with Rett syndrome as it is to girls. (If the boy has Klinefelter Syndrome then this approach is relevant to them as well.) RSRT’s goal of treatments and a cure applies to girls and boys with the disorder.
Although rare, males can have mutations in MECP2. There are three scenarios that may lead to males with Rett:
1) A boy has Klinefelter syndrome (which happens in 1 in 1,000 male births) and is born with an extra X chromosome (XXY). One of the X’s has the mutation and the other does not. These boys will have symptoms similar to girls with Rett.
2) A mutation derives not from the sperm or the egg but rather at a slightly later stage, such as the 20-cell stage (blastula). If one cell becomes mutated, every cell downstream to it will also mutate, while the remaining 19 cells and all cells that originate from them will not. This is called somatic mosaicism and the phenotype will resemble a girl with Rett, since the somatic mosaicism will function similarly to X inactivation patterns in girls.
3) A boy is born with a typical XY karotype and has mutations in MECP2 on all of his X chromosomes. Since he has no healthy copy to mitigate the mutated gene his symptoms are typically more severe than in girls. However, for reasons not yet understood, there are some boys with “milder” mutations.
MECP2 Duplication Syndrome
Unlike Rett syndrome, which is caused by mutations or deletions in the MECP2 gene and predominantly affects males, MECP2 duplication is caused by having an area of the X chromosome (Xq28), which includes the MECP2 gene, erroneously duplicated. The section duplicated varies between individuals and contributes to the severity of the disease.
The majority inherit the duplication from their mothers, who are typically asymptomatic due to favorable X chromosome inactivation (the moms have inactivated the X chromosome that harbors the duplication). These mothers have a 50% chance of passing on the duplication to their children.
MECP2 duplication syndrome may be quite prevalent. Preliminary studies suggest that 1% of cases of X-linked intellectual disability may be due to this syndrome. The core phenotypes in boys include infantile hypotonia, mild dysmorphic features, developmental delay, absent to minimal speech, recurrent infections, progressive spasticity especially of the lower limbs, ataxia, autistic features, and seizures.
Females with MECP2 duplication and without X chromosome inactivation, though extremely rare, have been reported to present similar symptoms to the males.
Family Testing
Should our Family get Tested?
Testing parents, siblings, and other relatives is a personal decision that each family must make. Family planning decisions can significantly influence whether parents should be tested.
The vast majority (99.5%) of cases of Rett syndrome are single occurrences in a family resulting from a sporadic mutation in a single sperm. Parents tested for MECP2 mutations almost always test negative.
In rare cases, however, the mutation comes from the mother’s eggs. Either of these two scenarios could occur would result in a 50% chance of a child inheriting the mutation from the mother:
- The mother’s eggs could have the mutation, known as germline mosaicism.
- The mother has the mutation in every cell, but due to favorable X inactivation skewing she does not have Rett symptoms. Again, an offspring would have a 50% chance of inheriting the mutation from its mother.
Testing the mother through a blood test would rule out skewed X inactivation, but the only way to detect germline mosaicism is by analyzing the eggs.
The father of an affected son does not need to be tested since boys inherit the mutated MECP2 gene from their mothers.
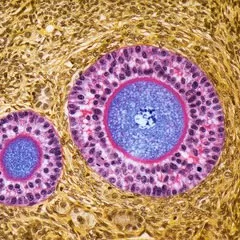
The mother’s eggs could have the mutation, known as germline mosaicism. An offspring would have a 50% chance of inheriting the mutation from their mother.
The mother has the mutation in every cell, but due to favorable X inactivation skewing she does not have Rett symptoms. Again, an offspring would have a 50% chance of inheriting the mutation from their mother.
Testing the mother through a blood test would rule out skewed X inactivation, but the only way to detect germline mosaicism is by analyzing the eggs.

The risk to siblings depends upon the genetic status of the parents.
When the mother of an affected individual is found to have the MECP2 mutation that was also identified in her affected child, the risk to siblings of inheriting the mutation is 50%.
If a mutation is not identified in a parent, the risk to siblings is low. However, germline mosaicism cannot be excluded.

Prenatal testing is available for parents who have a child with an identified MECP2 mutation. Prenatal testing is possible by analysis of DNA obtained between 15 and 18 weeks' gestation by amniocentesis, or chorionic villus sampling (CVS) between about 10 and 12 weeks' gestation.



